Mississippi’s health challenges are often framed as individual struggles. Eat better. Exercise more. Manage your stress. But for many families across the state, these messages ring hollow. They do not address the lack of access to care, the weight of chronic stress, the gaps in postpartum coverage, or the environments that make healthy living almost impossible.
During The Weight We Carry, a recent webinar hosted by the Foundation for the Mid South, health experts laid out a difficult but necessary truth. Mississippi’s health outcomes are not the result of personal shortcomings. They are the predictable outcomes of the systems people live within.
What emerged from the discussion was a portrait of a state where mental health, maternal health, and obesity are deeply interconnected, and where solutions must center on long term structural change, not short term fixes.
Stress, Biology, and the Hidden Drivers of Obesity
Mental health clinician Dr. Damien Thomas began with an explanation that challenged common assumptions about weight. Obesity, he argued, is inseparable from mental health, trauma, and chronic stress.
“When talking about serious mental illnesses such as schizophrenia, the prevalence of obesity is around 25 percent and combined weight obesity at 60 percent,” he said. The issue is not willpower. It is biology.
Thomas detailed how stress and depression trigger inflammation, disrupt hormones, and alter reward pathways in the brain. He explained, “We are talking about inflammation of various systems and how reward systems are being affected. As a result, individuals may have a tendency toward emotional eating.”
For many Mississippians, stress is constant, not episodic. Economic strain, caregiving demands, violence exposure, and community level trauma create a landscape where emotional eating is not a choice. It is a survival strategy.
His message reframed the conversation. Mississippi’s obesity crisis is not simply a public health issue. It is a mental health and structural inequity issue.
The Postpartum Gap That Puts Mothers at Risk
Maternal health advocate Whitney Hunter Batteast added another layer. She spoke with urgency about the lack of postpartum support, particularly for Black mothers.
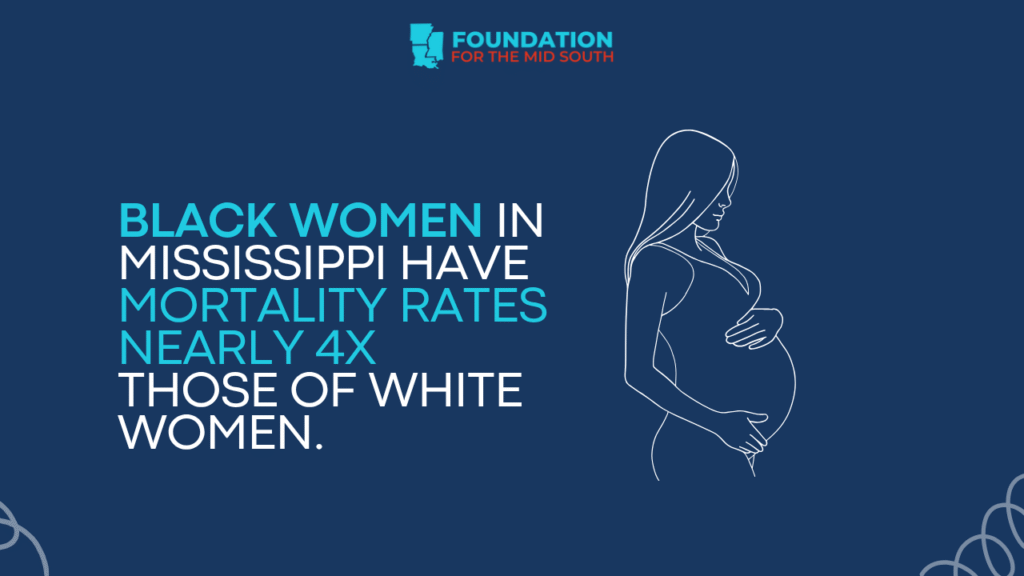
She was clear and direct. “Black mothers are four times more likely to perish than their white counterparts. And it is not because Black women do not take care of themselves. It is simply that we do not pay attention.”
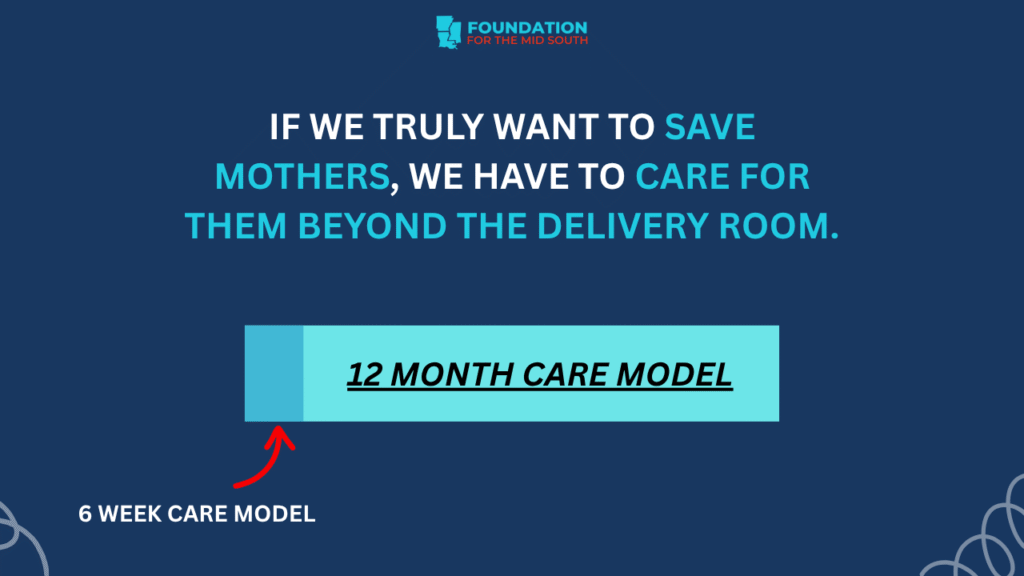
Hunter Batteast described a postpartum care system that expects women to recover from childbirth in six weeks and then disappear from the medical radar. She noted, “We stop thinking about moms after birth unless they are having a mental health crisis.”
The consequences are life threatening. Hypertension, depression, heart complications, and infections often emerge months after delivery, yet many mothers lose insurance coverage before they ever receive follow-up care. She emphasized how coverage gaps fuel crisis. “If you do not have coverage for a headache or a stomachache or chest pain, you cannot go to the doctor. That is where we fall through the gaps.”
Her comments illustrated how maternal mortality is rooted not only in medical care but in policy choices about coverage, access, affordability, and community support.
Obesity and Maternal Outcomes: A Policy Landscape in Need of Repair
Astria Goolsby, a public health leader at Family Health Center, walked the audience through the broader structural factors shaping obesity and maternal health.
She named the statistic many know but still struggle to grapple with.
“Mississippi leads the nation in obesity rates. We have seen the data. We see the evidence in our own communities.”
The problem is not lack of information. It is lack of access. “There are systemic barriers such as rural access gaps, food insecurity, and environments not conducive to physical activity,” Goolsby said. These challenges especially affect women of reproductive age, where obesity rates exceed 42 percent.
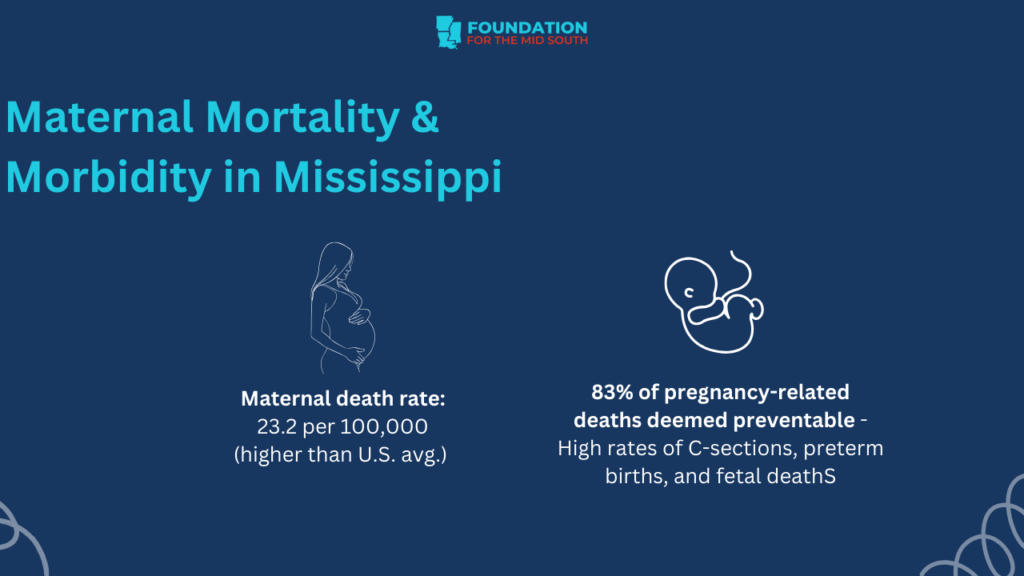
Goolsby tied these realities directly to maternal outcomes. More than 80 percent of maternal deaths in Mississippi are preventable, yet the policy, transportation, and cost barriers remain largely unchanged.
Her message was clear. To improve maternal outcomes, Mississippi must address obesity as a systems issue rather than an individual one.
The Real World Consequences for Families
Across the panel, a shared theme emerged. Families are carrying the consequences of underinvestment and fragmented systems.
Mothers ration medication because copays are too high. Individuals with depression struggle to access therapy. Rural residents must travel hours for basic care. Parents rely on emergency rooms for routine concerns because they cannot get appointments.
These conditions create downstream effects that no amount of personal behavior change alone can overcome.
Hunter Batteast described the contradiction many families face.
“On one hand, we tell moms here is everything you need to feel supported. On the other hand, there is a price list.”
The policies in place do not match the needs of the people who live under them.
Opportunities for Structural Change
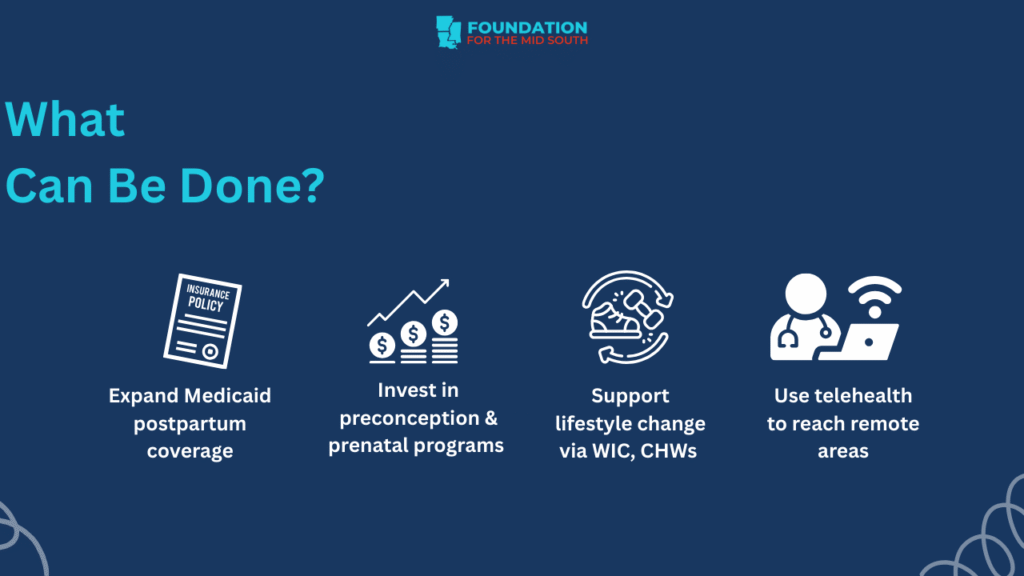
Despite the barriers, the panelists outlined clear pathways for systemic improvement.
Dr. Thomas pointed to the need for integrated care models. “We can offer co-occurring diagnoses and integrated treatment. That allows us to address both issues at the same time, which is best practice.”
Goolsby emphasized the importance of expanding mobile clinics and investing in community health workers who can identify local barriers and connect families to support. “We should invest more in community health workers and social service departments,” she said.
Hunter Batteast underscored the need for more accessible postpartum and peer support. “We are each other’s village,” she said. “If we collectively decide that a mom needs care, she needs various forms of care.”
The solutions are not theoretical. They already exist. What remains is scaling them.
Where the Foundation for the Mid South Fits In
The issues raised during The Weight We Carry align directly with the Foundation for the Mid South’s Health and Wellness strategic priority. The Foundation’s work focuses on:
- Increasing access to health services.
- Supporting maternal health and postpartum care.
- Advancing trauma informed practices.
- Strengthening community-based prevention efforts.
- Reducing systemic barriers in underserved areas.
These goals reflect the urgent needs identified by the panelists and offer a roadmap for meaningful progress.
A Path Forward for Mississippi
The Weight We Carry highlighted a difficult but hopeful truth. Mississippi’s health outcomes are not fixed. They are the result of decisions, investments, and policies that can change.
Families across the state are carrying more than they should have to. But as the panelists made clear, the weight becomes manageable when communities are supported, when systems function equitably, and when policymakers understand the realities of the people they serve.
Mississippi is at a crossroads. The data is clear. The stories are real. The solutions exist. The question is whether the state will take the collective steps needed to build a healthier future.
The work has already begun. And the weight can be lifted.
Explore the Webinar
Real change starts with understanding the systems shaping our lives. We encourage you to watch the complete webinar and join the ongoing conversation about building healthier, more equitable communities across Mississippi.
Watch the replay: The Weight We Carry